Addendum to What the DSM-5 Gets Wrong About Mental Illness
Responding to questions on my previous post
My latest essay (see here) generated some interesting discussion on Reddit about the Hierarchical Taxonomy of Psychopathology (HiTOP), much of which concerned the HiTOP’s relevance as a clinical tool. Firstly, thank you to all who commented! It allows me to improve my own understanding of this stuff, and helps me to see gaps that I might have missed. I appreciate it.
Also, a special thanks to maybeiamwrong2 for drawing my attention to this review article, which I had previously missed. I highly recommend it to interested readers if they want a more detailed and up-to-date overview of the HiTOP.
The HiTOP is pretty interesting in its own right, but it’s central to my own project here, so I thought it would be worth doing a follow up post to address some of the main questions and comments that arose.
Clarifying the HiTOP’s method for ‘diagnosis’
ScottAlexander:
How does HiTOP prevent us from pathologizing ordinary behavior? If we wanted to pathologize homosexuality we could just put it in Internalizing->Sexual Problems->Homosexuality, and then it would be just as pathologized as if we called it 303.1: Homosexuality or whatever in the DSM.
How does HiTOP help us treat human traits in a less binary way? I agree it's a judgment call whether to diagnose someone with depression. How is it any less of a judgment call whether to diagnose someone with Internalizing->Distress->MDD?
Yes, many conditions are comorbid and it's hard to draw lines between them. How does renaming GAD to Internalizing->Distress->GAD and OCD to Internalizing->Fear->OCD make their comorbidity less awkward than it is in the DSM?
Yes, two people can be diagnosed borderline with only one symptom in common. How does renaming it Antagonistic Externalizing->Borderline help solve this?
My goal with ‘What the DSM-5 Gets Wrong About Mental Illness’ was to provide a relatively accessible introduction to the HiTOP. Unfortunately this meant cutting some of the more technical details of the model, but I believe the HiTOP developers do address most of these issues.
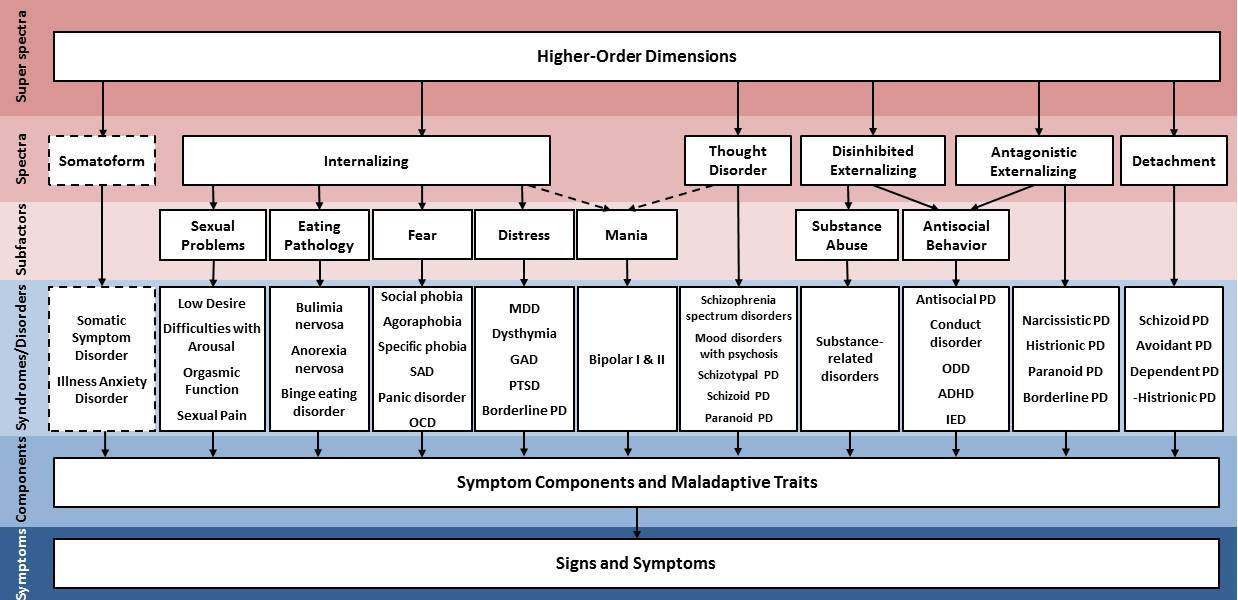
The HiTOP was not specifically designed as an alternative to the DSM-5, but it has come to be something entirely different. In the 2017 article, the diagram includes the DSM-5 diagnoses as part of the model:
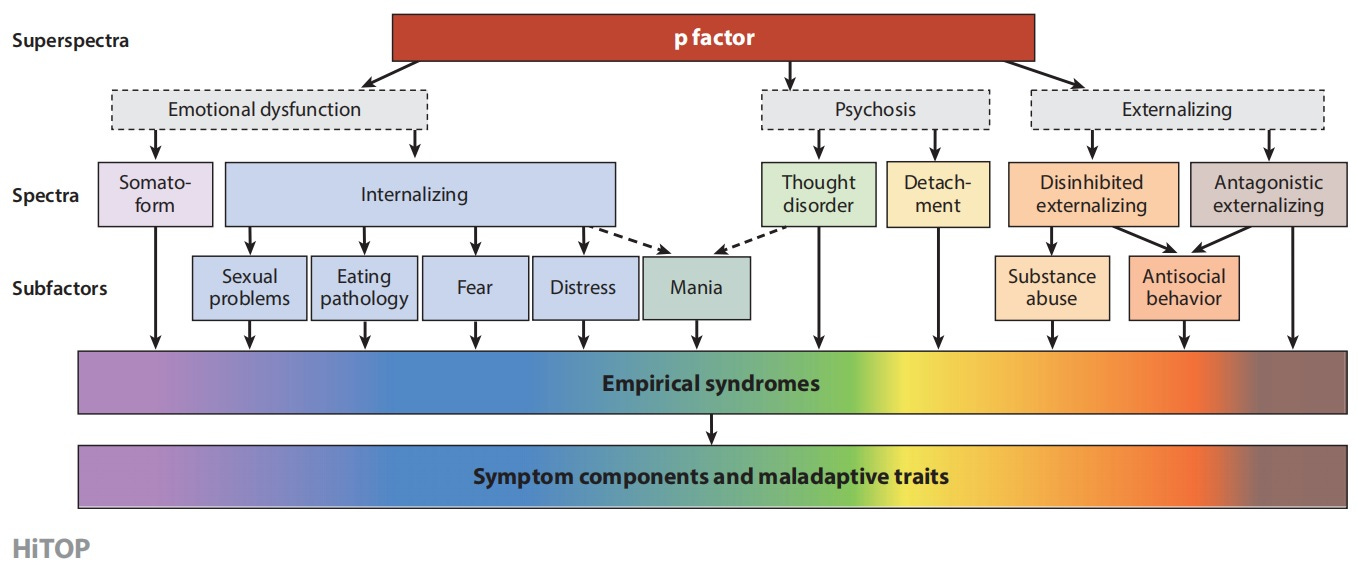
This is a bit of a misrepresentation. Their intention was to provide an indication of where the HiTOP dimensions cross over (empirically) with traditional diagnoses, not to suggest that assessment of psychopathology via HiTOP would include a DSM-5 diagnosis. The 2021 article maybeiamwrong2 shared fixes this:
What this tells us is that (for example) Eating Pathology is more likely to co-occur with other Internalising subfactors like Fear than with Antisocial Behaviour, and Antisocial Behaviour is more likely to co-occur with other Externalising subfactors like Substance Abuse than with Fear. All might be present, of course, but if short on time a HiTOP-informed clinician could use this knowledge to target their questions in a useful way.
Digging deeper, someone with with Anorexia Nervosa (AN) may not always actively meet criteria for this diagnosis. Fairburn et al.’s transdiagnostic theory of eating disorders suggests that there are several features core to most eating disorders (certain cognitive distortions, behaviours, etc.), and in practice, people who present with eating disorders often cycle between them over time. This pattern is essentially what the Eating Pathology subfactor represents. In my own practice I’ve found this very helpful—when a previously anorexic client wonders why she has developed a habit of binge eating, I can explain this cycle and target the core underlying issues, rather than treating this as a new and separate diagnosis.
So in essence, my response to all of these questions is that the HiTOP is an entirely different system to the DSM-5. When it comes to diagnosis and the potential for stigma, there are no labels—instead, a unique trait profile of the person is developed that places them on a series of sliding scales. We all sit somewhere on these scales, and being higher or lower on a particular trait isn’t necessarily cause for concern until it becomes a source of distress or significant impairment. This is where clinical interviewing comes in. The clinician can then explore a person’s individual difficulties and see whether they match up with a person’s HiTOP profile. In many cases they will, but not always; for example, there are many people who experience mild schizotypy symptoms who interpret these through a spiritual lens, and thus feel no distress over them.
Dimensions vs categories
maybeiamwrong2:
As far as I am aware, the HiTOP does not assume dimensionality. So if there was good taxonomic evidence of categories, they would implement them as such.
Yes, the HiTOP is intended to be an atheoretical, empirically-derived model. It doesn’t assume that psychopathology is inherently dimensional, categorical, or otherwise. However, the research to date largely supports the dimensional approach, so the HiTOP is made up of predominantly dimensional, transdiagnostic constructs. That said, the authors make clear that this does not preclude the inclusion of categorical constructs in future if the data support this: “HiTOP is not wedded to any single method or type of construct and can evolve to include, for example, nondimensional constructs… should evidence for such constructs emerge” (DeYoung et al., 2021, p. 3).
Ok-Tank5893:
On your categorization angle, definitely agree, the fact that the personality disorders are clustered based on superficial similarity is huge. Why not get rid of the category and just rename each disorder? for example obsessive compulsive personality disorder, completely different, not even on the spectrum of actual OCD, but confusingly named like it.
True enough about the confusing nature of some DSM-5 labels. I think the answer to this problem goes back to the HiTOPs approach to ‘diagnosis’, which is to say, the HiTOP doesn’t diagnose—there are no labels as such, only dimensions upon which we all sit.
HiTOP and the Big Five
Ok-Tank5893:
Does HiTOP map with the big five personality traits? I’ve seen research where you can actually express most diagnosis as extremes / dysfunction in those areas (which is sort of a hindsight explanation of therapy benefits but it does offer a useful map)
maybeiamwrong2:
The DSM-5 Alternative Model of Personality Disorder might have deserved a mention, as well as the more dimensional ICD-11 (compared to both the ICD-10 and DSM-5). All three map pretty neatly onto each other and the Big Five.
I received a couple of comments highlighting the overlap between the Big Five/Five Factor Model, the DSM-5 Alternative Model of Personality Disorder, and the HiTOP. I discussed the FFM in part 1 of this series, and this was no coincidence—all three models seem to be mapping the same 5-6 core traits at different levels (of severity? Rigidity?). The HiTOP Consortium have themselves acknowledged this overlap many times, e.g., in the 2021 article: “[the Big Five] may be considered individual differences in psychological functions, and abnormalities in any of them fall within the scope of HiTOP” (p. 19.12), “These [Alternative Model of Personality Disorder] dimensions form the core of five HiTOP spectra, which include traits—alongside signs and symptoms—that are very similar to AMPD traits” (p. 19.13). This is something I intend to discuss further in part 3.
On the ICD-11—an earlier draft of my essay did reference the ICD, but I decided to remove discussion of this for the sake of brevity and focus. In my (admittedly limited) understanding, the ICD has made strides toward a more dimensional approach to conceptualising psychopathology, but is not all the way there yet. I’ll look more into this, and perhaps do a separate post on it in future.
Abstracting away from clinical usefulness
ScottAlexander:
It might help if we frequently thought of things on a higher level than the end diagnosis, but this sounds dangerous - I actually care a lot whether someone has ADHD vs. Antisocial Personality Disorder, and as long as those are in the same bin I am not going to be thinking in terms of bins any more than I am already. Same with OCD vs. panic disorder - these have very different therapies and treatments.
wizard_of_autumn:
I wonder if they don't abstract too much, for a crude example afaik social phobia is usually a feeling of inferiority, internalised as social fear. For me, under the HiTOP, the connection of specifically inferiority being internalised as social phobia get's lost a bit, as it looks like any stressor could be internalised as any symptom, while some stressors are usually much more likely to take a specific expression as a symptom. That's just speculating from a layperson tho.
Both of these comments point to one of the biggest hurdles facing the HiTOP. I largely agree—it’s one thing to build ever more accurate models, it’s another to implement them. The DSM-5 currently has the advantage in this regard. It allows for quick and easy transmission of key information about a person’s mental health issues, which can then be acted on by other professionals. This might mean for treatment—where, as Scott noted, there are specific treatment approaches known to work for specific disorders—but is also important in other areas. To use an example from my own country, having a clear mental health diagnosis makes accessing funding under Australia’s National Disability Insurance Scheme (NDIS) much easier. It would be unreasonable to expect a non-expert to attempt to interpret a full HiTOP profile to assess funding eligibility, so psychologists and doctors would shoulder the burden of additional assessment and report writing to fill this gap.
A solution may one day be found for this problem, but for now, I think the best we can hope for is a system in which the HiTOP and DSM share space in the clinical realm. Bureaucracies love labels, and therapists are wary of them—we’ll just have to find a happy middle.
(This is an addendum to part 2 of a 3 part series On Personality and Psychopathology. Part 3 can be viewed here.)